What is Lyme Disease?
Lyme disease is spread through the bite of an infected tick. The disease is caused by Borrelia Burgdorferi, a tiny bacterial cork-screw shaped spirochete. These spirochetes can be passed from an infected tick to humans through a single bite. The longer a tick is attached, the more likely it is to transmit the diseases it is carrying to you.
According to the Centers for Disease Control and Prevention, Lyme disease is the fastest growing vector-borne infectious disease in the United States. The CDC estimates that 476,000 people in the U.S. are diagnosed with Lyme disease every year. Lyme disease affects people of all ages. Children ages 4-14 are most at risk. Adults ages 60-79 also are at high risk.
Disease Transmission
Lyme disease is spread through the bite of an infected tick. Ticks feed on blood. When a tick takes a blood meal, it can transmit the pathogens it has in its gut to you. Some diseases can be transmitted faster than others. There continues to be disagreement about the time it takes for Lyme disease to be transmitted, ranging from 18 hours (ticklab.org) to 48 hours. Some infections, such as Powassan Virus can be transmitted in as little as 15 minutes, and Rocky Mountain Spotted Fever (Rickettsia Rickettsii) can be transmitted in 6 hours.
Given the possibility of rapid transmission, removing an attached tick as soon as possible can reduce your chance of getting sick from a disease the tick may be carrying.
THE LONGER A TICK IS ATTACHED, THE GREATER THE PROBABILITY OF DISEASE TRANSMISSION.
In addition, many people are not aware they’ve been bitten by a tick and may not make a connection when they begin to experience symptoms, which can occur weeks, or even months after a tick bite.
REMEMBER: there are other infections you can get from a tick bite that can be transmitted more quickly than Lyme disease. Do not assume there is zero risk because a tick wasn’t attached for 24 hours. Consider tick testing (ticklab.org) to determine attachment duration and pathogens the tick may be carrying.
REFERENCES:
Ticklab.org - Diseases Transmitted by Blacklegged (Deer) Tick Bites
Dr. Cameron - https://danielcameronmd.com/long-take-infected-tick-transmit-lyme-disease/
Early Transmission Possibilities:
Nymph Bites: Studies, including those from the Institut Pasteur, suggest that nymph bites, especially those involving European species of B. burgdorferi, can lead to transmission within 12 hours.
Matuschka and Spielman Study: Research by Matuschka and Spielman indicated that about 5% of infected Ixodes dammini nymphs transmitted B. burgdorferi within the first 24 hours of attachment, with about 50% transmitting it after 2 days.
Lyme borreliosis: a review of data on transmission time after tick attachment
Mechanisms for early transmission of spirochetes have been proposed based on their presence in different organs of the tick. Studies have found systemic infection and the presence of spirochetes in the tick salivary glands prior to feeding, which could result in cases of rapid transmission. Also, there is evidence that spirochete transmission times and virulence depend upon the tick and Borrelia species. These factors support anecdotal evidence that Borrelia infection can occur in humans within a short time after tick attachment.
Early Signs & Symptoms
Initial symptoms may occur within a day or a week, and often people think they just have the flu or virus. But some patients may present with only neurological symptoms. “Summer flu” is highly unusual – and healthcare practitioners are informed to consider Lyme and Tick-borne diseases when patients experience a “summer flu-like illness.”
Rashes: bull’s-eye or red expanding rash, irregular rash (scroll down to next section for more detail on rashes)
Flu-like symptoms: fever, chills, sore throat, swollen glands, nausea, muscle aches, joint pain
Bell’s palsy, facial muscle weakness or paralysis
Sleep disturbance
Headaches (may be severe)
Fatigue
Lightheadedness, fainting, shortness of breath
Heart palpitations or chest pain (Lyme carditis)
Neck stiffness
Shooting pains that may interfere with sleep
Swollen lymph nodes
Pain and swelling in large joints
Night sweats
If you are experiencing any symptoms after a tick bite, be sure to reguarly take your temperature. Lyme disease often does not cause a fever, but some co-infections may cause fever spikes, or a low-grade fever. Write down any symptoms you have, educate yourself by reading current articles about the disease, and get to a health care practitioner.
For a more comprehensive checklist of rashes and symptoms by tick-borne diseases, check out our Dare to Know Insert (free to download and print).
Later Signs & Symptoms
If the initial infection goes undiagnosed and untreated the infection can progress, disseminating throughout the body, and affecting any organ.
In the heart, the bacteria may cause heart block or palpitations. Recent reports of sudden cardiac death due to Lyme carditis highlight the importance of prompt diagnosis and treatment of Lyme disease.
When the bacteria affects the digestive system, patients may experience nausea, acid reflux, irritable bowel syndrome, poor digestion, or diarrhea.
Endocrine disturbances such as hypothyroidism or menstrual irregularities are common.
In the brain, Lyme disease may cause learning disabilities, memory impairment, headaches, sleep disturbances, and concentration problems often presenting like attention deficit disorder (ADD).
There may also be joint swelling and pain, muscle soreness, twitching, and cramps.
Some experience light and sound sensitivity.
Most patients with Lyme also have fatigue, which can be quite debilitating.
For a more comprehensive checklist of rashes and symptoms by tick-borne diseases, check out our Dare to Know Insert.
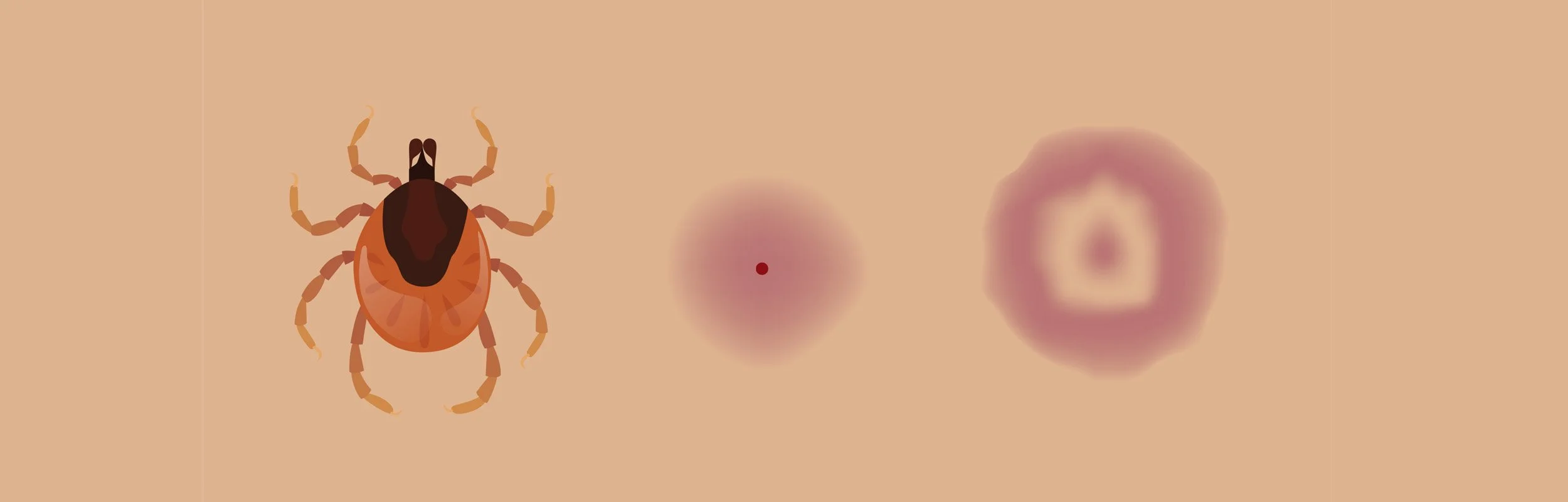
Tick Bite Rashes
BULL’S-EYE / RED EXPANDING RASH:
The most common early sign of Lyme disease is an EM (Erythema Migrans) rash.
It starts as a reddened area at the site of a tick bite.
It often expands over days or weeks, sometimes developing a bull's-eye appearance with a red ring around a clear center.
EM is caused by the bacteria that causes Lyme disease, and it usually appears 3-30 days after a tick bite.
NOTE: Not everyone gets a rash with a tick bite. In positive Lyme cases, patients often do not recall having a rash.
In Pennsylvania, getting an EM rash is diagnostic (positive) for Lyme disease and should be treated immediately; no test required.
IRREGULAR RASH:
A tick-bite rash doesn't always present as a well-formed bull's-eye.
It can be irregular, vary in appearance, faint or difficult to see.
Do not dismiss an irregular or faded rash.
When a rash spreads, it shows Lyme infection spreading in the body; treatment is needed as soon as possible.
The rash may feel warm, usually not painful, and could expand reaching up to 12 inches across.
In some cases, multiple EM rashes can appear on different parts of the body, indicating a disseminated infection.
photo credit: Lymedisease.org
NO RASH:
Some people do not get a rash with a tick bite. In positive Lyme cases, patients often do not recall having a rash.
REGARDLESS of if you get a rash or not …
If you suspect you have a Lyme disease rash, it's important to see a doctor for diagnosis and treatment. ILADS guidelines indicate physicians should prescribe 4-6 weeks of antibiotics for patients with a bull’s-eye rash.
Tick-Borne Disease Diagnosis
Lyme disease is a "'clinical" diagnosis determined by a physician relying on their experience in diagnosing tick-borne diseases. Testing is an adjunct to their clinical diagnosis. See testing information. A negative test CANNOT rule out Lyme disease. Many physicians use a checklist of Lyme symptoms, employing clinical assessment and testing to rule out other diseases. Check out our Dare to Know insert, free to download and print.
Symptoms can change quickly and come and go (first it's headaches, then joint pains). Because ticks transmit multiple co-infection diseases, many symptoms overlap with Lyme, and some are quite unique which can help in the proper diagnosis.
Lyme disease often mimics the symptoms of other diseases. Misdiagnoses include Chronic Fatigue Syndrome, Lupus, Rheumatoid Arthritis, Fibromyalgia, Alzheimer’s, ADD/ADHD, Autistic-Spectrum Disorder, Psychiatric illnesses such as Depression and Anxiety Disorder, and Neurological illnesses such as Multiple Sclerosis, Parkinson’s and more.
Many of these diseases do not have gold-standard tests, which means that a Lyme disease evaluation relies heavily on the medical practitioner’s clinical judgment, knowledge, and experience with Lyme disease.. When appropriate, a Lyme literate practitioner will use specialty laboratories when ordering blood tests to diagnose Lyme disease.
Ticks can also transmit multiple diseases. Therefore, when being evaluated for Lyme disease, patients should also be evaluated for other Lyme strains e.g. Borrelia miyamotoi, and common coinfections like Anaplasmosis, Bartonella, Babesia, Ehrlichia, Mycoplasma, Q Fever, Rocky Mountain Spotted Fever, Tularemia and more. Some of these symptoms overlap with Lyme, and some are quite unique, which can help in the proper diagnosis.
Lyme is Frequently Misdiagnosed
Lyme disease is a multisystem illness and can affect various organ systems, including the skin, joints, heart, and nervous system. Lyme disease is known as the “great imitator.” Over 150 common Lyme symptoms are core symptoms of other diseases. It takes a skilled medical practitioner to recognize the patterns of what may seem like unrelated symptoms to make a diagnosis of Lyme disease. Lyme disease is frequently misdiagnosed as:
Alzheimer’s disease
Amyotrophic lateral sclerosis (ALS)
Attention deficit hyperactivity disorder (ADHD)
Carpel tunnel syndrome
Chronic Fatigue Syndrome
Depression
Fibromyalgia
Lupus
Multiple Sclerosis (MS)
Parkinson’s
Psychiatric illness
Rheumatoid arthritis
Temporomandibular disorders (TMJ)
Psychological Aspects of Lyme Disease and Tick-Borne Diseases
This video, originally created for the PSEA (Pennsylvania State Education Association), provides an excellent discussion on the psychological aspects of Lyme Disease and other tick-borne diseases. This educational video is ideal for school nurses, doctors, parents, and anyone who wants to learn more about the psychological components of Lyme Disease (particularly in children).









